There are major changes for everyone who uses tearzipitide as part of a weight loss journey. In a move that made waves in the health care industry, CVS Health recently announced that it would remove the “zipbound” CVS Kermark Formulary, effective from July 1, 2025. This means that CVS Health will not cover the terozptide for weight loss under its insurance plans. However, CV will cover Weagovo In its formulas, Novo is a rival GLP-1 drug through Nordsesk.
This decision has given rise to substantial conflicts using patients Zipbound for weight lossTheir CVS Carmerk is covered through a plan, now they may have to face more out -of -pocket costs.
This change does not just affect which drugs are covered. This can affect your tearzipitide weight loss treatment, monthly costs and even your health journey.
So, why is the CV making this change? And what does this mean for patients and payers (employers and insurance providers)? Let’s find out.
What is Terzepatide and how does the weight loss work work?
Terzepatide sold as a zipbound, is a GLP-1/GIP receptor egonist that helps people lose weight. Approved by the Food and Drug Administration (FDA), Terzptide is one of the most interactions Weight loss medicines Due to its powerful consequences in clinical trials.
|Also Read: Weight Loss with Seminary or Terzepatide: Which works better?|
Why did the CVS dropped the trispatide?
Although the reasons for preventing covering of weight loss are not stated, it seems that the move is the leading prices and costs behind the curtains.
Pharmacy Benefit Managers (PBM), such as CVS Kermark, are conducting a permanent review of drugs based on their medical effects, prices and discounts. When many medicines fall into the same category, Zipbound and Vigo, PBMS, compete against cheap prices, which can happen this time.
What does this mean for patients
If you are currently taking weight loss L -Terzptide and your health plan is through CVS Kermark, you need to know that:
1. You have to pay the maximum price
The zipbound will be transferred to a non -preferred or non -covered status, which means that you may have to pay the entire retail price for the tractoid treatment, which can exceed $ 1,000 a month.
2. You may need to turn to Vigovo
The CVS is still covering Vigo, another GLP-1 drug. Talk to A Certified Obesity Medicine Physical from the BoardFor, for, for,. Like Dr. Mona Lala, to check whether to switch to Vigo or other GLP-1 drugs is suitable for your health needs.
3. You may need permission before
If you are medically necessary to treat tearzipitide, your weight loss doctor may have to file an appeal or ask for permission before. But these processes may be timely and do not guarantee approval.
What will be the effect of this decision?
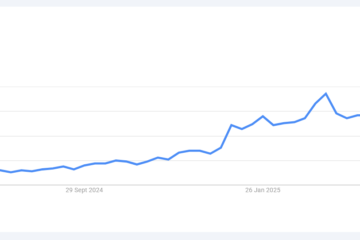
The CVS’s decision to quit the Terrorism from its formula may be more than just a business call – how to manage weight loss medicines through insurance companies and PBMs can be a sign of extensive changes. As the use of GLP-1 medicines for weight loss The concern about their growing cost of insurance companies is increasing. PBMs, such as CVS Carrmark, are feeling the pressure of either banning access or attacking better price deals with manufacturers.
But many patients not only see GLP-4 as weight loss tools, but as a way of better health, especially for people who are suffering from obesity conditions. Therefore, any move to restrict access, such as the recent CVS decision, is likely to push through weight loss -tero -tiletide users.
Pharmaceutical companies have also begun to find alternative ways to reach patients. This can mainly change how the method of distributing and covering medicines is changed, making it difficult for PBM to control access as in the past.
Is the GLP-1 drug landscape changing?
Yes, faster
GLP -1 drugs such as zipbounds, Vigo, and Ozampak are no longer just diabetes medicines. They are becoming the focus of how we treat obesity, heart disease and other health conditions.
But they are also very expensive, and insurance is trying to overcome the spending costs. If you are planning to take or take these medicines for weight loss, expect to see:
- More first options
- Formulary Exception (Like it)
- Step Therapy, where patients try cheap medicines first
Patients, weight loss advisers, and pharma companies will need to navigate this evolutionary landscape carefully.
What can you do if you are affected?
If you are currently taking weight loss LZ zipbound or tarziptide and insured through CVS Carramark:
- Talk to Your weight loss doctor has a safe and efficient option for you to discover the skin.
- Call your insurance provider and ask about options, appeals, and will the zipbound be included in any capacity.
- Check out Eli Lily’s Patient Aid Programs Help the price if you qualify.
- Insurance policies change. Keep an eye on the CVS, your HR team, or your insurance provider’s updates.
Remember, you have options, and the initial action is key. Talk to your doctor, ask tough questions, and don’t be afraid to advocate your health.
Need to navigate your coverage or seek options?
Schedule the consultation With Dr. Mona Lala to support your care and coverage management in the world of changing health care.

0 Comments